For decades, scientists have been trying to find cures for all the various cancers that plague humanity and have made incredible strides towards this goal. We currently have various treatments that are able to significantly prolong survival and in some cases completely treat the cancerous tumor. One of the major roadblocks in our ability to cure this disease is related to the incredible heterogeneity that exists within each tumor and each patient. Additionally, the way each organism responds to the tumor cells is also extremely varied placing a lot of pressure on clinicians and scientists to constantly adapt.
One such promising therapy involves using immune checkpoint inhibitors (ICIs) which are currently approved to treat a variety of cancer types, including breast, bladder, cervical, colon, liver, lung and more.
Immune checkpoints are a normal part of the immune system.
Immune cells are our bodies’ defense mechanism, tasked with identifying and eliminating harmful foreign organisms or diseased cells such as tumor cells. Immune cells are generally very good at their job, so good that sometimes their response can be too strong resulting in the destruction of perfectly healthy cells.
Immune checkpoints are triggered when proteins on the surface on T cells (a type of immune cell) bind to proteins on other cells sending an “off” signal to the T cell so that it doesn’t destroy our own healthy cells.
Tumor cells hijacked this system and express these proteins on their own surface, thus tricking the immune cells into believing they are good cells that don’t need to be destroyed. One such example is the pair of proteins PD-L1 which is expressed by the tumor cells and its partner PD-1 expressed by T cells. When they bind each other, T cells back down and don’t destroy the cells expressing PD-L1. ICI therapies work by blocking this interaction in tumor cells, allowing the immune cells to recognize and destroy them.
Tumor cells can evade immune cells by expressing PD-L1
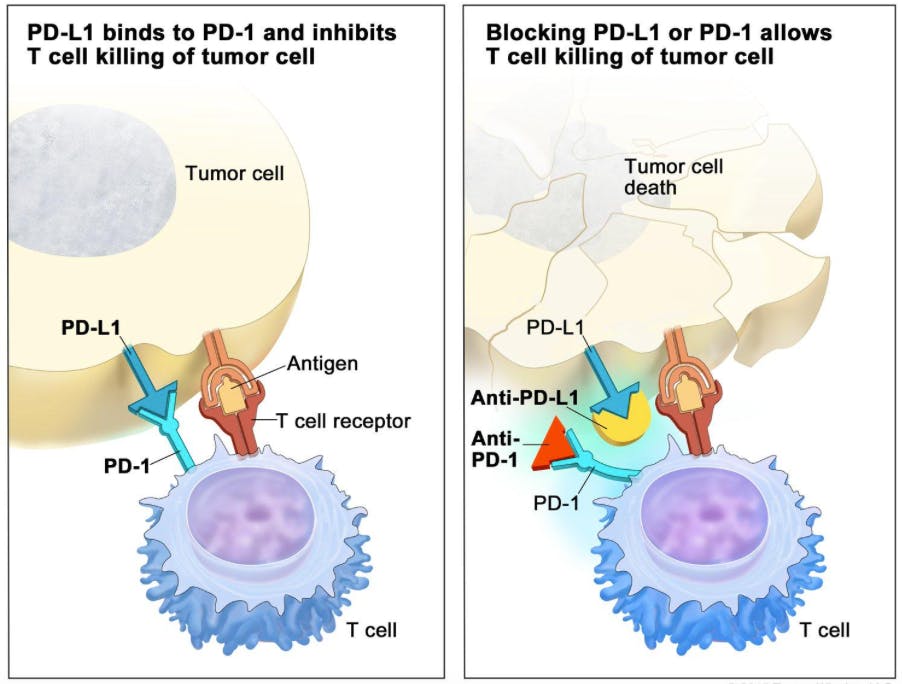
Interaction between PD-1 and PD-L1 results in immune evasion. Blocking antibodies disrupt this interaction allowing tumor cell death to occur. Source: National Cancer Institute.
ICI treatment has been proven effective in a subset of patient tumors that are correlated with activated T cells, but a large variety of patients remain unresponsive to this therapy. To try and enhance this response and help a higher number of patients, combinations of different ICIs have been used, however toxicity levels are extremely high, highlighting the need for better strategies.
To address this shortcoming, a team of scientists from Merus NV biotechnology company in the Netherlands recently published their findings of a bi-specific antibody that potently activates CD137 via engagement of PD-L1 to enhance tumor specific T cell responses. CD137 is a protein expressed on the surface of T cells when they become activated.
Expressing CD137 ligand on the surface of tumor cells has been shown to result in tumor elimination making CD137 a great candidate for ICI therapies.
There are currently two CD137 agonist antibodies in clinical trials, urelumab (IgG4) and utomilumab (IgG2) however, results from both have been less than ideal. This need is what lead to the unbiased screening performed in this study which identified MCLA-145 as a potent activator of T cells by binding to CD137 and PD-L1 either separately or together.
MCLA-145 is a CD137xPD-L1 bi-specific antibody with great therapeutic potential
Excitingly, the team found that MCLA-145 potently activates T cells, promotes immunological memory and overcomes immunosuppression by tumor cells. They found that in a T cell priming assay using primary T cells, MCLA-145 was able to potently activate T cells with both an effector and memory phenotypes in 4 donors (Fig 3a).
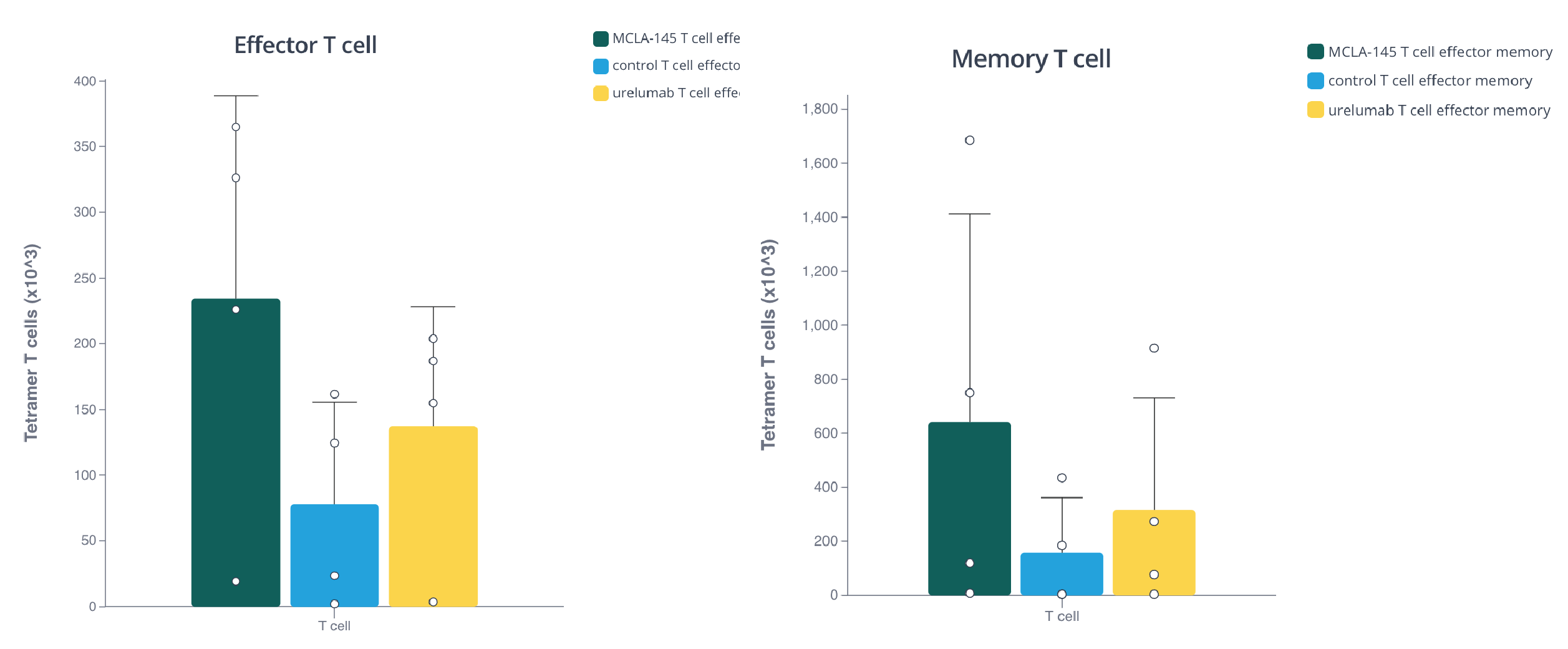
Barplot showing the effect of MCLA-145 on effector and memory T cell priming from 4 donors. Plot made with Pluto.
Additionally, MCLA-145 was able to elicit great cytokine production levels in a transactivation assay using purified T cells from 7 donors. (Fig3b) and it was able to stimulate IFNγ and TNFα in memory T cells, whereas urelumab had no effect (Fig 3e).
Cytokine expression indicates T cell activation

Box plot shows cytokine expression induced by MCLA-145. Plot made with Pluto.
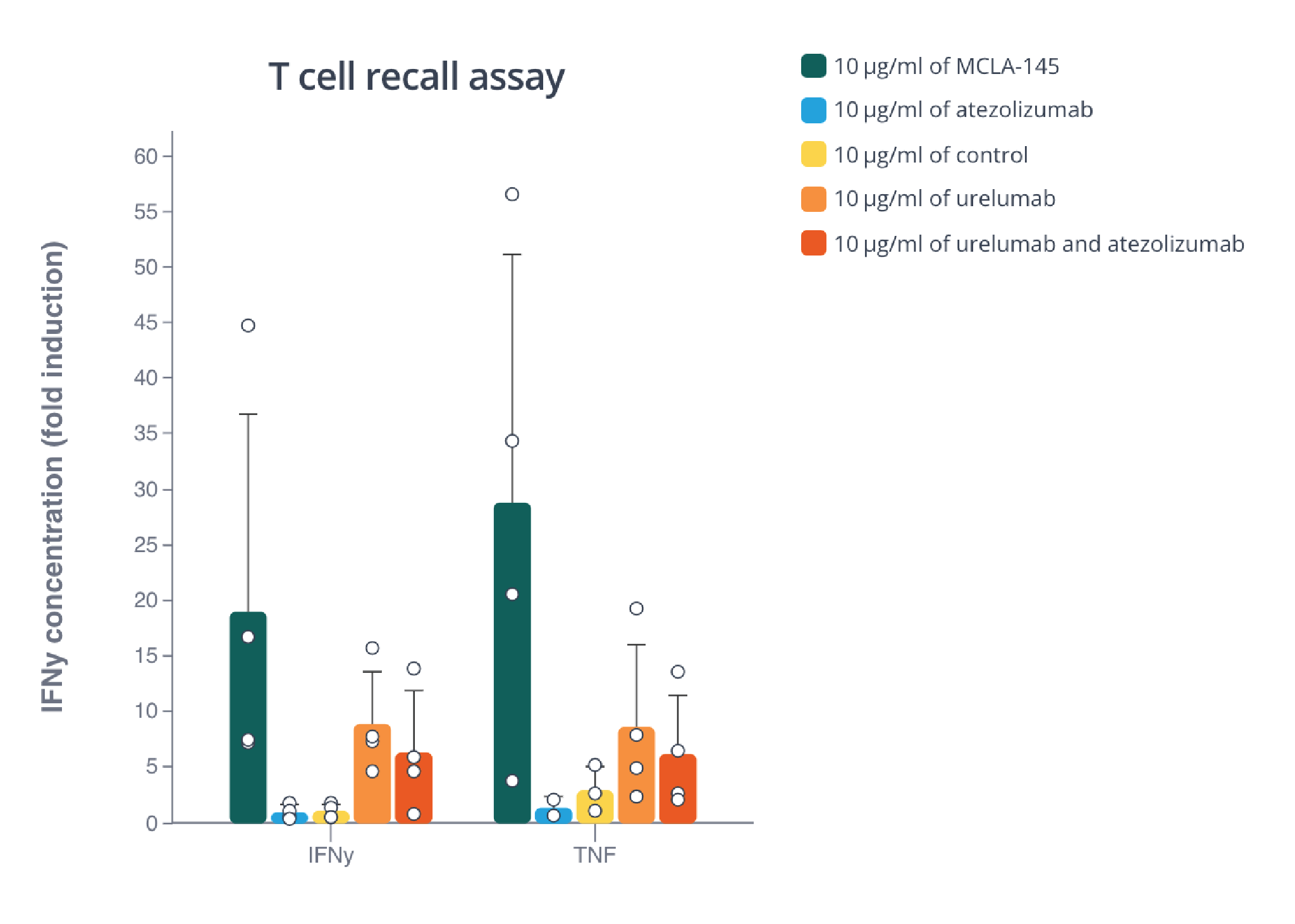
Memory T cells are potently activated by MCLA-145 as seen by the high cytokine levels. Barplot made with Pluto.
The ability of MCLA-145 to activate multiple subtypes of T cells is crucial for its potential success in the clinic. The different T cell types are like different branches of the military, the more we can send into battle, the better chances of survival we have.
To investigate the activity of MCLA-145 under more therapeutically relevant conditions, the team used fresh tumor explants from 5 primary endometrial tumors. Treatment with MCLA-145 increased the levels of IFNγ production relative to control in all tumor samples. However, the results were variable between the different tumors, highlighting the previously mentioned difficulties in finding ubiquitous successful treatments for all patients due to the varied response within each patient.
Every patient has a slightly different tumor and every organism behaves in its own unique way. This is just one of the many puzzles clinicians and scientists are working to solve in the fight against cancer.
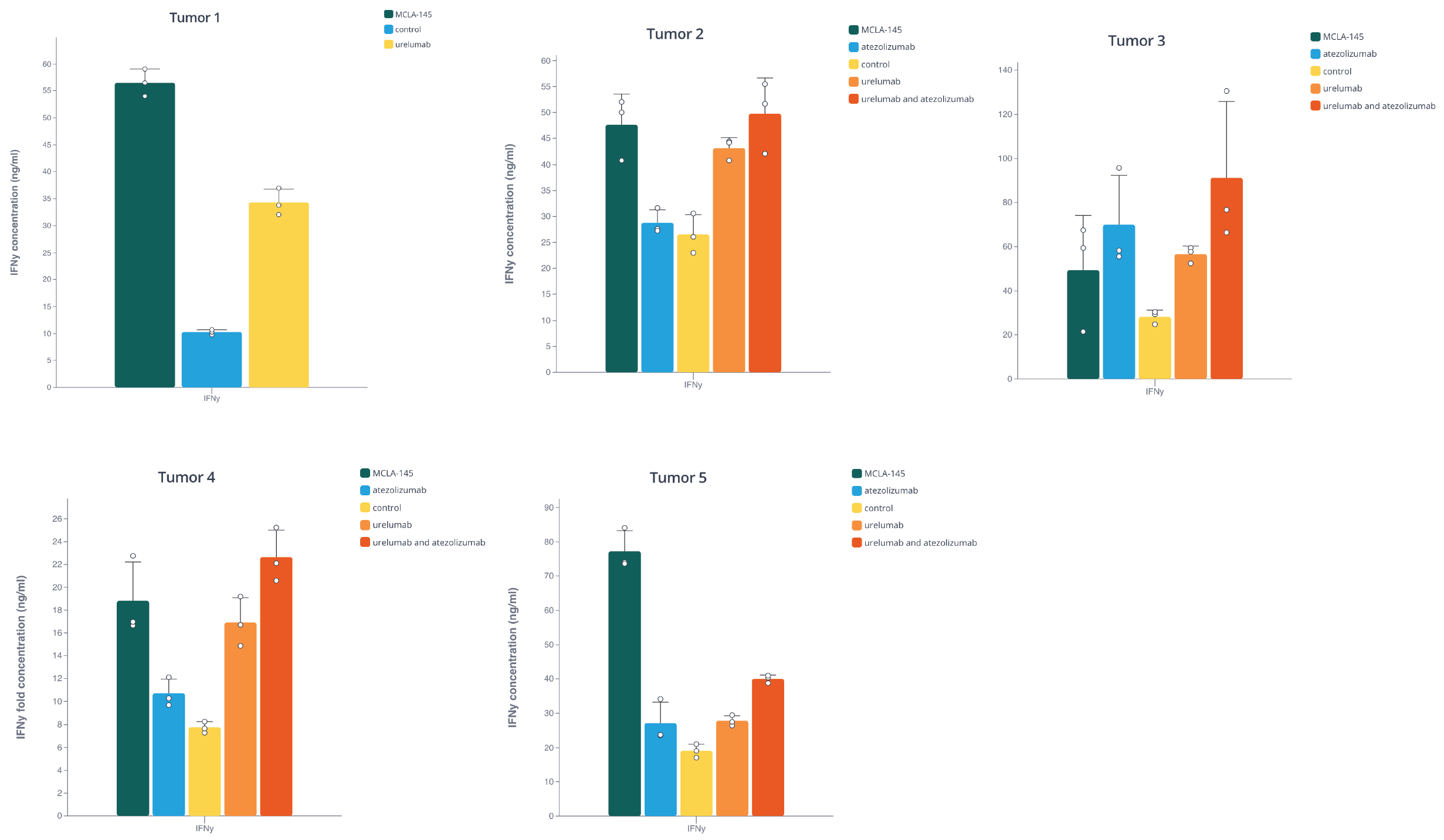
MCLA-145 induced IFNγ expression above the control levels in 5 primary tumor samples. Barplots made with Pluto.
Due to the previously reported side effects of ICI combination treatments, the team wanted to ensure that MCLA-145 was well tolerated in non-human primates at high doses. They found that even at the highest dose of 100mg/kg, MCLA-145 was well tolerated with no changes in organ weight, no gross or microscopic pathological findings identified. Blood chemistry and liver enzymes were also all within normal ranges, suggesting that MCLA-145 is well tolerated even at doses that are 1000 times higher than the safest urelumab dose of 0.1mg/kg. This is the first report of a fully human cross reactive CD137 agonist successfully tolerated at this dose level and it suggests that MCLA-145 will have a favorable safety profile in humans.
Based on data from this study, MCLA-145 can be expected to serve as either a mono therapy in cases where ICI treatments fail to improve patient outcome or as an adjuvant to boost responses to other treatment modalities such as cancer vaccines or chemotherapy. MCLA-145 is currently being evaluated in an open label, dose-escalation single-agent study with expansion cohorts for dose confirmation/safety and preliminary efficacy in advanced or metastatic malignancies (NCT03922204).
References
Geuijen, C., Tacken, P., Wang, LC. et al. A human CD137×PD-L1 bispecific antibody promotes anti-tumor immunity via context-dependent T cell costimulation and checkpoint blockade. Nat Commun 12, 4445 (2021). https://doi.org/10.1038/s41467-021-24767-5.
“Immune Checkpoint Inhibitors” overview published by the National Cancer Institute here.
Pluto ensures that you not only have fast and reliable results so that you can continue to push the boundaries of knowledge, but that those results are also easily accessible, shareable and publishable right from your browser. Ready to give it a try? Contact us to schedule a personalized demo for your lab.
