Pluto Bioinformatics
GSE132732: Human interleukin-4 treated regulatory macrophages promote epithelial wound healing and reduce colitis in an mouse model
Bulk RNA sequencing
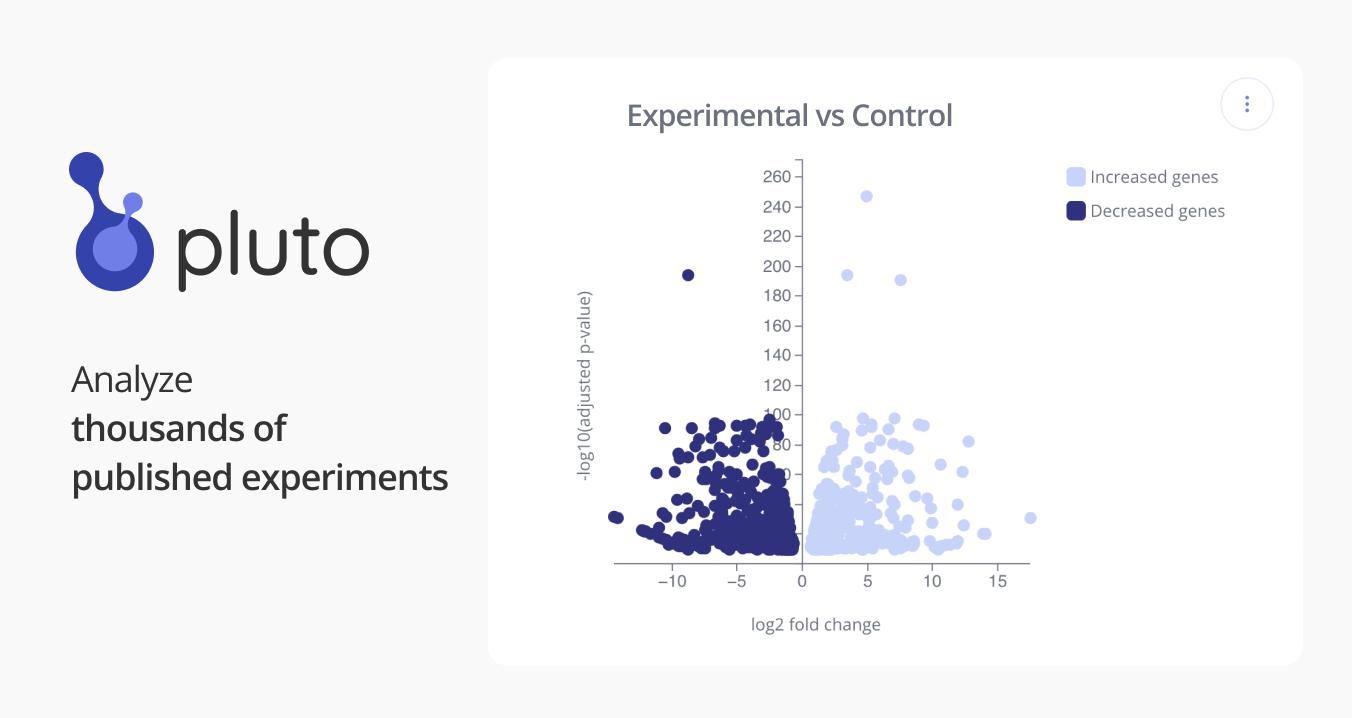
Murine alternatively activated macrophages can exert anti-inflammatory effects. Expanding upon this, we sought to determine the ability of human IL-4-treated macrophages (i.e. hM(IL4)) to promote epithelial wound repair and serve as a novel anti-inflammatory cell transfer treatment for inflammatory bowel disease (IBD). Blood monocytes from healthy volunteers and patients with Crohns disease or ulcerative colitis (active and inactive disease) were converted to macrophages and treated with IL-4. Subsequently, cells were assessed by qPCR, in in vitro epithelial wounding and permeability models, and for anti-colitic capacity in dinitrobenzene sulphonic acid (DNBS)-treated Rag1-/- mice. IL-4 treatment of blood-derived macrophages from healthy volunteers and patients with inactive IBD resulted in a characteristic CD206+CCL18+CD14low/- phenotype (RNA-seq revealed IL-4 affected expression of 996 genes). Conditioned media from freshly generated or cryopreserved hM(IL4)s were equally effective in promoting wound healing, and reducing cytokine-driven loss of epithelial barrier function in vitro. Systemic delivery of hM(IL4) to DNBS-treated Rag1-/- mice significantly reduced disease as assessed my macroscopic disease and histopathology scores. Remarkably, the anti-colitic effect of hM(IL4) transfer was still apparent when mice were challenged with DNBS one month after receiving hM(IL4)s. Positing that hM(IL4)s would be anti-colitic, this study demonstrates the capacity of M(IL4)s from healthy volunteers and patients with inactive IBD to promote epithelial recovery after injury and to suppress colitis. These novel findings with hM(IL4), provide proof-of-concept support for the development of autologous M(IL4) transfer as a cellular immunotherapy for IBD. SOURCE: Matthew Workentine University of Calgary